Sunday, March 9, 2014
Welcome to Memoirs of a Warrior
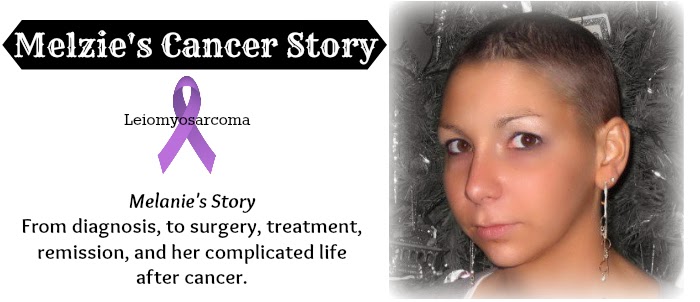
This is a website dedicated to my cancer journey, which began in late 2005 and continues to this very day.
I am a Leiomyosarcoma Survivor.
I was unexpectedly diagnosed in February 2006 after undergoing surgery to remove my {then thought to be benign} tumor.
Following a long and difficult recovery, I underwent intense treatment to attempt to rid my body of any remaining cancer cells.
On November 20, 2006, I received my first clear scan and was officially in remission.
Since then, I have been dealing with many, many complications caused by my surgery and treatment. Life is far from easy and I'm continually trying to find new ways to adjust to my ever changing body.
Please feel free to explore my website.
If you have any questions, please do not hesitate to email me or comment on any of these pages. I am 100% comfortable sharing my story, answering questions, and talking about my journey.
My reason for sharing my story is to touch, inspire, and relate to others.
When I went through my difficult battle, I felt lost and alone. I had no one to turn to that could fully understand what I was going through. I searched the internet looking for others I could contact; other young adults going through what I was going through. I wasn't very successful but the few I found helped me out tremendously. I share my story in the hopes that another young cancer patient will stumble upon and find solace and comfort in reading my story. I encourage anyone to reach out to me for support. I reached out to others and now I am paying it forward.
Tuesday, March 5, 2013
My Cancer Story
Like everyone, I have my own story to tell. No two stories are alike. What I experienced as a cancer patient was and is much different than any of the people sitting in a chemo pod next to me. Thankfully, my story is one of success. I'm here today to tell you about my story and I am forever grateful for this second chance at life. That's not to say my journey was easy. It was far from that. And on many days, I still suffer from side effect that cancer left behind.
I enjoy talking about my story. While it's incredibly difficult at times, I like to share my story for various reasons. I love to share my story in the hopes of giving someone else hope. During my cancer days of diagnosis, surgery, and treatment, I felt lost and alone. I was 21 and felt like I had no one who truly understood what I was going through, emotionally and physically. I turned to the internet. I found other young adults' blogs. I found comfort in reading their stories; the good and the bad. The bad scared me, but it also prepared me for the rough road ahead of me. The good gave me hope. I was determined to live the positive life they led. I promised myself I too would win my battle just as they had done. Reading their blogs let me know my fears about the unknown in my health, even after many years in remission, is normal; that I'm not the only one walking around in constant fear and worry. My hope is that someone else will stumble upon my blog and find this same sense of comfort and hope. That they too can feel they have someone who understands. My hope is that this is a place they can come to read about endoscopies, surgery recovery, coping with diagnosis, what to expect with treatments and how life after cancer is. That their fears and emotions, even many years past, are normal.
I also blog to raise awareness. I want people to see the rawness and hardships this awful disease can bring about. That it can strongly affect one's life. And that even though treatments have ended, survivors still need love and support. Finding and adjusting to a new normal in life, accepting a changed body, coping with fear of relapse, and dealing with the after affects of cancer are all difficult. We still struggle on a daily basis. Some more than others. I hope that by sharing my story, I can touch people to fight for a world without cancer. That people will join more organizations such as Relay for Life (or any other cancer related fundraiser) to raise money for research and programs to help cancer patients and their families; to volunteer to help others suffering from cancer. I want to inspire people to fight for a cure and help those suffering in any way.
Links found below are currently inactive as their pages undergo construction
- 21 March 2014
About Leiomyosarcoma
I enjoy talking about my story. While it's incredibly difficult at times, I like to share my story for various reasons. I love to share my story in the hopes of giving someone else hope. During my cancer days of diagnosis, surgery, and treatment, I felt lost and alone. I was 21 and felt like I had no one who truly understood what I was going through, emotionally and physically. I turned to the internet. I found other young adults' blogs. I found comfort in reading their stories; the good and the bad. The bad scared me, but it also prepared me for the rough road ahead of me. The good gave me hope. I was determined to live the positive life they led. I promised myself I too would win my battle just as they had done. Reading their blogs let me know my fears about the unknown in my health, even after many years in remission, is normal; that I'm not the only one walking around in constant fear and worry. My hope is that someone else will stumble upon my blog and find this same sense of comfort and hope. That they too can feel they have someone who understands. My hope is that this is a place they can come to read about endoscopies, surgery recovery, coping with diagnosis, what to expect with treatments and how life after cancer is. That their fears and emotions, even many years past, are normal.
I also blog to raise awareness. I want people to see the rawness and hardships this awful disease can bring about. That it can strongly affect one's life. And that even though treatments have ended, survivors still need love and support. Finding and adjusting to a new normal in life, accepting a changed body, coping with fear of relapse, and dealing with the after affects of cancer are all difficult. We still struggle on a daily basis. Some more than others. I hope that by sharing my story, I can touch people to fight for a world without cancer. That people will join more organizations such as Relay for Life (or any other cancer related fundraiser) to raise money for research and programs to help cancer patients and their families; to volunteer to help others suffering from cancer. I want to inspire people to fight for a cure and help those suffering in any way.
Links found below are currently inactive as their pages undergo construction
- 21 March 2014
About Leiomyosarcoma
Radiation
Chemotherapy
Remission
Remission
Life After Cancer
Sunday, March 3, 2013
Leading Up to My Diagnosis
In November 2005, I was experiencing some abdominal pain. It wasn't too concerning, but I visited the Student Health Center at Mizzou. Without running any tests and just listening to my symptoms, the doctor said I probably had IBS (irritable bowel syndrome). I was confused because I wasn't experiencing diarrhea, as I associated with IBS, but she said it can just cause cramping and pain in the abdomen. I went on my way and things seemed to improve throughout the month.
I remember at Christmas that year, I wasn't feeling too well. I wasn't necessarily sick, but my body just didn't feel right. I was slightly nauseous but not enough that I couldn't keep food down, and I ate Christmas dinner just fine. I just didn't eat a lot and afterwards, I didn't feel too great.
I had a headache but it wasn't even strong enough that I took Tylenol.
I remember thinking I was showing signs of the flu. But it never came.
I just wasn't my normal loud and obnoxious self.
None of this seemed too alarming to me.
Throughout December, I was also starting to lose energy. As the month passed, I grew weak and fatigued. Very normal activities would cause me to be out of breath. I often found myself incredibly winded after making my bed. I'd have to sit down and catch me breath.
On Friday, January 6, 2006, back in Columbia, Missouri at my duplex (where I was attending Mizzou), I was putting clothes from my washing machine into my dryer. I had to take a break because I felt like I was going to pass out. My roommate and best friend from high school, Jessie, finally convinced me to go to the Student Health Center. I, and others who knew my symptoms, were convinced I had mono. It was running rampant around campus so it was highly possible. And it made sense. It was the only thing we could think of that made you feel like crap and made you so weak and fatigued for weeks on end while also giving you the sore throat I was experiencing.
I headed to Mizzou's Student Health Center and because it was winter break, I was seen pretty quickly. I told the doctor everything that had been going on and she agreed that it sounded exactly like mono. She informed me it was a simple blood test and they'd call me with the results when they were in. They drew some blood and sent me on my way home.
Right as I was walking in the door to my duplex, I received a call from my doctor. She told me that my blood counts, specifically my hemoglobin, was dangerously low. She commented that she didn't know how I wasn't passing out from all the activity I was doing with my hemoglobin at 5 (the norm is 13). {For those that do not know, your hemoglobin carries the oxygen.} She then said that I needed to go straight to University Hospital because I was being admitted. She informed me that I would probably need a blood transfusion and then we'd need to figure out where or why I was losing blood.
I was shocked. I began tearing up. I had never, ever been in the hospital. Not even the ER. Honestly, the last time I was in a hospital (not a regular doctor or Urgent Care) was when I was born! I'd never broken a bone or had a severe illness. The worst thing to ever happen to me was the flu every few winters. I was a healthy, very active athlete. How could this be happening?? Until this day, I had been a very, very healthy individual. What had changed? I was so scared with so many questions running through my brain.
Thank goodness Jessie was home. She drove me to the hospital and I called my mother on the way. She immediately hopped in the car and headed from St. Louis to Columbia. I don't think anyone has ever driven those two hours any quicker than she had.
We arrived at the hospital, I checked in, and was taken up to a hospital room. They immediately began running some tests and I honestly don't even remember what all it was. I just remember how terrified I was. And confused. I felt like crap, but definitely not crappy enough to now be in a hospital gown, lying in a hospital bed. My mother finally arrived and a while later Jessie left (she had called into to work and told them she'd be late. I cannot thank her enough for how amazing of a best friend she was (and still is), especially because hospitals and all bodily type things and needles really freak her out.)
The nurse then informed me I would be getting a blood transfusion to replenish my body of the blood it lost. She began attempting to insert an IV into my hand. At this point in my life, I did not like needles and this was very uncomfortable for me. She had a difficult time, moving the needle all over under my skin, hoping to get the flashback of blood to let her know it was inserted correctly. I'm not too sure what happened because I was not looking at my hand, but I suddenly hear the nurse saying "Oh my gosh, it's going to explode!" in a frantic voice. I look down and see that the back of my hand had ballooned up and (because I'm an idiot), I clearly thought she meant my hand was going to explode. Thankfully, that was not the case, it was only the vein in which she placed the IV, but it was still painful and not a pretty sight for the next two weeks.
Thankfully, an IV tech came in and placed a new IV into my elbow pit (clearly I'm not knowledgeable on proper terminology.) Once the IV was in, they began my first blood transfusion. It took about four hours for the first bag and immediately after the blood transfusion, they took some blood and tested it. It showed my hemoblogin had risen to somewhere around 8.
A few hours after the blood transfusion, they took my blood again to test my levels and see if it was holding steady. My hemoglobin had begun to drop again. So we knew I was losing blood somewhere. The weird thing was, I was not vomiting up blood, nor did they detect any in my urine or stool samples.
A while later, a nurse came in and talked to us (us now being my mother, brother (who also lives in Columbia), and I). She began talking about the probable causes for blood loss: tear in my esophagus, a bleeding ulcer, or blood cells splitting. I didn't think twice about this because I didn't know what it meant. That is, until I heard my mom talking quietly to my aunt mentioning this, and crying. I could sense something was wrong. Eventually my brother convinced my mother to tell me. Apparently "blood cells splitting" is a strong indication of Leukemia. I asked the nurse and she confirmed that's what she meant and said that Leukemia is actually common in women in their early 20's. I was terrified. Cancer? There was no way. That couldn't be me they were talking about. I've always been so healthy! She informed me that they were going to be running a test to check for this and I should know within a few hours what the next steps were. I was terrified. I laid there for the next few hours fearing I had cancer; a thought that, up until this point, had never, ever crossed my mind.
Because I was still losing blood, I had to get another blood transfusion. So they hooked me up and began running another bag through me.
Somewhere in this time, another blood test was run and it confirmed my blood cells were not splitting, and therefore I did not have Leukemia. I was so happy. We were all so relieved to know I didn't have cancer. Huge sighs of relief and tears of joy were shared. Little did we know, Leukemia probably would have been the much better option. Who would have thought that I should have hoped it would be Leukemia?; That the end outcome was going to be much worse than Leukemia.
I was then (wrongly) discharged from the hospital. After my first blood transfusion, I was told I could not go home if my levels were not holding steady and they were not at least at 10. I was at 8.9 and they wouldn't send me home. Then after my second blood transfusion, they checked my levels. And then again in a few hours. They had dropped and I was at 8.7 And they discharged me. They discharged me when my levels were still dropping. They discharged me at a lower hemoglobin rate, 8.7, than half a day before when they wouldn't discharge me with the 8.9. We know it's simply because they were packed. They had people on beds in the hallway waiting for rooms. They simply got rid of me to make more space. We were mad, but at the same time, I was happy to be back home in my own bed, in real clothes, with no machines beeping 24 hours a day, and IVs stuck in my arm.
I was sent home after 48 hours in the hospital with orders to go to the Student Health Center on Monday (it was now Saturday evening) and get my blood drawn to see how my blood levels were. I was also scheduled for an endoscopy there in Columbia to check for a bleeding ulcer or tear in my esophagus about two weeks later.
I was also told that I was anemic so I needed to consume things with a lot of iron (recommended more red meat) and I was also prescribed iron supplements.
My mother stayed with me through the weekend and that following Monday, I returned to the Student Health Center to get my blood checked. Good news! My blood levels had risen from my hospital stay. It meant that I wasn't losing blood and that my body was now producing more to replenish my lost supply.
Mom took me shopping and made sure I was stocked on healthy red meats. Then she headed back home to St. Louis and would return for my upper endoscopy.
Fast forward two weeks and my Mom arrives and we head to University Hospital for my endoscopy. I had never had one done before so I was a little nervous. I didn't need to do anything on my part. Just don't eat after midnight the night before, show up, remove my belly button ring, and answer a lot of questions.
Next thing I knew, I was being told to count backwards from 10. I made it to 9 and that's all I remember.
I then woke up in recovery and my mother was there. I asked her about the endoscopy and she said they did figure out where I was losing blood. She told me that I had "bleeding mass" in my stomach, about the size of a golfball. It was a large mass (they weren't yet calling it a tumor) located up near the opening of my esophagus and the bottom of it was ulcerated and bleeding.
Unfortunately, they were not able to biopsy the mass. They were afraid if they cut into it, it might bleed too much. They said it would be best to schedule a surgery and just get it removed.
Because of an amazing nurse, we did not get the surgery scheduled in Columbia. After the doctor told my mother what he had found and that I would need surgery, a nurse approached her. She told my mother that she hadn't seen anything like this, nor had that doctor, and she needed to take me home. She told my mom I needed experts and that since we're from St. Louis, she should take me home to be seen by a doctor at Barnes-Jewish Hospital/Washington University, one of the top hospitals in the nation (ranked within top 10 for gastroenterology and cancer.)
By this time, classes had started again. I took time off at the end of January to head home to St. Louis and have another endoscopy done by the doctor who did my father's surgery when he had ulcers. Unfortunately, he was also not able to biopsy the mass. After the endoscopy, he was 100% honest with my family and told them that this was far beyond his area of expertise, but he highly recommended Dr. Battafarano at Barnes Jewish Hospital.
He made a referral for us and we scheduled another endoscopy with him. At this point, my tumor was no longer bleeding so they were able to biopsy it and they told us it was benign. Thank goodness, right? Not cancerous!
Dr. Battafarano then set us up with an amazing doctor, Dr. Linehan, to schedule surgery and get the mass removed. My original surgery was not scheduled until April but thankfully, he called at the beginning of February to say he had an opening on February 14, 2006. We jumped at the opportunity. The sooner we could get it out, the better.
Saturday, March 2, 2013
Surgery, the Hospital Stay, and Diagnosis
Before my surgery date, we had an office meeting with Dr. Linehan. He talked about the surgery and what all would be done.
He informed us that he would most likely have to crack my chest and that he would be removing my entire stomach. He would then cut a piece of my small intestine or colon and create a stomach out of that. It was a rare surgery but he is one of the top in the nation and we trusted him. He briefly mentioned I'd be on bedrest for a while after surgery but never really mentioned just how painful recovery would be.
Late afternoon on February 13, 2006, my brother, sister, and I all piled in the car and headed to St. Louis. I remember my mother being so mad because we got on the road much later than we planned, and I needed to be home to drink my nasty drink to completely clear out my digestive system.
We arrived home around 8pm, I drank my drink, and honestly, didn't expel of much like I was told I would.
I went to sleep that night without a care in the world. I really wasn't concerned. I didn't think I needed to be. My tumor was benign and for some reason, I was under the impression this was going to be a simple surgery. Looking back, I'm not at all sure why I thought this. Had I not heard the doctor say they were going to crack my chest and remove my stomach? Honestly, I think I was just relieved to know my tumor was benign so nothing else seemed to matter to me. I was just ready to get it all over with. Little did I know that this was my last night of lying down without worrying. Little did I know from that night forward, I'd worry so much.
The next morning, we headed to the hospital. My surgery wasn't slated until about 2pm that afternoon. I was shocked when shortly after arriving at 8am, they called my name to go up to pre-op. I wasn't expecting it. My siblings, Ben and Leah, had stopped at another hospital to see my Grandma who had just had a total knee replacement. They weren't there to see me off.
My mother asked if they could go with me and the staff said no. (Looking back, I'm not sure why. I went to the exact same pre-op I have been going to for years now afterwards for my endoscopies and they ALWAYS let someone come with me.)
My mom and dad teared up, hugged me tight, told me they loved me, and that they'd see me soon. I remember feeling weird. Should I be crying? My parents are. They seem so worried. Should I be? Have I been in denial over what's really happening? Maybe I didn't prepare for this like I should have. As I was walking back to the elevator to be taken up to pre-op I became so scared and sick to my stomach. I suddenly realized this was a bigger deal than I thought. I wasn't going in for a simple surgery. My parents were crying for a reason. And I was now alone.
In pre-op, I was overwhelmed. I had never been in this situation. They asked me so many medical questions. I didn't have a medical history prior to this. And everything in the past few weeks was new and confusing. I didn't even know the answer to half of the questions. I wanted my parents with me so badly. I needed their help with these questions. I changed into a gown, and was hooked up to an IV. I had a ridiculous amount of doctors and nurses and PAs coming in. My surgeon came in, then his residents, then his nurse, then his physician's assistant. Then the anesthesiologist came in, then their nurse, then their residents. So many people. All asking the same questions. And everyone was just so interested in my rare story. After the fourth "You're too young to be going through all of this", I started to get anxious out of fear of what "this" was.
Thankfully, I began to calm down as I realized I was in very good hands. All the questions were answered, urine sample given (they refused to believe I was a virgin and demanded a pregnancy test. I guess it's hard to believe a 21 year old is still a virgin these days???) I was just chilling in the bed, wrapped in blankets, with saline running through my body.
Then the anesthesiologist came in. They asked if I wanted an epidural. 'Epidural?? I'm not having a baby' I thought. Until this point, all things health and medical were not interesting to me. Actually, all things medical related made me queasy. I had only ever heard of an epidural in relation to pregnancy. I had no idea that it blocked pain. (Looking back, I was stupid. I should have known that but it just goes to show so how far removed I was from this all.) When they asked, I looked at them, with a terrified face, and said "I don't know. Do I need one?" The anesthesiologist's face instantly changed demeanors, as if saying "this poor girl" and she grabbed my hand and said very slowly and softly, "Honey, you're getting a very major surgery. I'm sorry there's no one up here with you, but yes, I would highly, highly recommend an epidural." I began crying, agreed to the epidural, and signed a form after being read the risks involved. Then they came in, told me to sit up, swing my legs off the side of the bed. They brought over a table, placed a pillow on top, and told me to lean forward over the pillow. I saw the ginormous needle and began (internally) freaking out. It hurt so badly!!!!!!! I began crying and asked if there was any way my mom could come up. Unfortunately, we were close to surgery time so they said no. (I've never seen more people look so sorry for something than the staff did for me on that day.)
Shortly after, an anesthesiologist came in and said they were going to give me something to relax me and then I'd be taken back to the operating room. Whatever they gave me made me feel drunk. But definitely relaxed. Things became a blur. I remember being wheeled down the long hallway into the OR. At this point, I was out of it enough that I couldn't open my eyes or speak, but I could still hear things around me and was conscience of what was going on.
They peeled off my gown, exposing my entire front side down about 6 inches past my belly button. They began cleaning my entire body...my neck, my entire chest, my stomach, and down past my belly button. I remember being so incredibly cold (those ORs are FREEZING to begin with. Then add in the fact that you're now wet and fully exposed, it's horrible.) They then just stood around talking, leaving me exposed (they couldn't cover me up because they had just sterilized my entire body) for what felt like 10 minutes. I felt so awkward. Just lying there, face up, topless, freezing cold. Finally, I heard Dr. Linehan enter. They placed a mask on my face, the anesthesiologist then said they were going to give me the drug to knock me out and asked me to count backwards from 10. I made it to 8 and I was out.
The surgery took about 6 hours. Afterwards, Dr. Linehan came down to the waiting area and pulled my family into a consult room. (At that time, my mother, father, brother, sister, grandpa and a few aunts and uncles) were all there. He explained that the surgery went well and because the tumor was encapsulated, he was able to save two-thirds of my stomach and only removed the very top third, plus the very bottom of my esophagus. I was also fortunate that he was able to work around my ribs and they did not have to be cracked. Then came the bad news. He told my family that the pathologist would confirm it, but their original tests were wrong. My tumor was in fact malignant. They were also informed the tumor, in just three short weeks, had grown from the size of a golf ball, to the size of an orange. (I cannot imagine how large it would have been if we had not been offered this cancelation in his schedule and kept our original April date.)
I had been cut from just below my sternum, down to about an inch-and-a-half above my belly button. I had a feeding tube on my right side that went directly into my small intestine. I had a drain on my right side (I'm not sure where it went into. I'm pretty sure it was my stomach.) Thankfully, Dr. Linehan had an AMAZING resident working with him, Dr. Doyle. She asked Dr. Linehan if she could stitch me up herself, explaining that I was far too young, with far too nice of stomach to have a big ugly scar. She took her time and spent more than double the time that most people would take to stitch someone up.
I was in recovery in the ICU. I will say that I do not remember much of my first 9 days (of 14) that I was in the hospital. I have very few, very blurry memories. My first memory, I was lying in the bed, not too long after surgery, and I could sense an elephant in the room. Even though I was told before my surgery that my tumor was benign, I could sense that had changed. I asked my brother, "Do I have cancer?" To which my mother responded "Yes." And then I freaked out. Sobbing. My machines all started going crazy and the nurses had to come in and calm me. I cannot imagine being my family, having to find this out, then tell me, and watch my reaction, while already watching me in so much pain.
During these first three days, my pain was not manageable. When the doctors would ask on a pain scale from 1 to 10, with 10 being hit by a semi-truck, how did I feel, I would always say a 10. I was always crying. Always in so much pain. I was on the highest dose of pain medication. They could not give me anymore without me becoming toxic. My original surgery was on Tuesday and just a few days later on Friday, Dr. Linehan decided to take me back in for surgery. He said there was no reason I should still be in that amount of pain and I could possibly have an infection or something such as a sponge may have been left in me.
Thankfully, after reopening me, they saw nothing. Dr. Linehan flushed me out, added another drain to my side, and I was closed back up. Again, Dr. Doyle took her time stitching me up. I cannot thank her enough. I've seen too many scars in my days (many of them other places on my body now) and they look large, rough, puffy in places. The scar on my stomach looks absolutely amazing. Honestly, I don't know that for as large a cut as was made, that it could look any better. I truly appreciate her genuine character for wanting to do this for me. I am very insecure about my scars, especially that one, but I cannot imagine how much worse it would be had any other doctor stitched me up.
Anyway, this second surgery seemed to do the trick because my pain had receded so much compared to the previous few days.
Dr. Linehan told us they thought my tumor was a GIST (gastro-intestinal stomal tumor). This was actually good news. With the cancers it could be, this was the best one. It was simply treated with a Gleevac pill, with none of the typical side effects of cancer (nausea, hair loss, fatigue, etc). And these cancers very rarely come back. We were very relieved to hear this and just needed to wait for the final pathology report to confirm it, before beginning treatment.
As I said, I do not remember much of my first 9 days in the hospital. I was not allowed to eat or drink ANYTHING. I wasn't even getting anything put into my feeding tube. I was simply living off whatever was going into my IVs. My mouth was so dry. My family members were allowed to wet a sponge and move it around my mouth to moisten it. I would cheat and squeeze it with my tongue and cheek to drink the water. But the moment it went down, the drains sucked it right out. It was frustrating because I just wanted to drink.
We also realized, while in ICU, that I am allergic to morphine. It causes itching and hallucinations. So much so that I was injuring myself. I would think I was a rollercoaster and it was headed for a wall, so I would jump out. But in reality, I was sitting up (using my abdomen which wasn't allowed) and trying to jump out of bed. My hallucinations kept causing me to move around which then caused a large deal of pain for me, and also caused me risk of injuring my surgery site. I was quickly taken off that.
Another side effects of the pain medicine was that it made me see things. They weren't hallucinations, more so just effects of the medicine. And they didn't cause me any physical pain. For instance, I would tell my brother that there were dinosaurs in my room. In reality, they were just flowers in vases. One time, I began swatting at the air asking my best friend, Jessie, "Do you see that?!" I thought I saw something falling all around me, and was swatting at it all. Another time, I yelled at my mother that someone was trying to come in the door behind me, when in fact, there was no door behind me, only a wall. Another time while Jessie was there, I was yelling at our cat, Mike Jones, to leave me alone. Jessie kept telling me he wasn't there but I saw him and he was bothering me. Thankfully, my family and friends saw humor in all of this.
In the hospital, I was not allowed to use my abdomen. At all. I just laid there in bed. After I was out of ICU, I began physical and occupational therapy. Physical therapy first started with learning to sit up. I had to grip the side rail of the bed with my arm, pull myself on my side, then push myself up with my arms, then lift my legs off the side of the bed. It might sound easy but it was so incredibly hard. You never truly realize how much you rely on your abdomen until you're not allowed to use it. Then I would learn to stand. Then to walk.
Occupational therapy worked with me to learn to put my socks on (another very difficult task since I was not allowed to bend over). They taught me how to use the restroom and how to do my breathing exercises.
Oh those breathing exercises. I hated them. I refused to do them. Essentially, I had this apparatus.
I had to put my mouth on it, suck IN and raise that bottom yellow part to a certain point, continuing suck in to hold it there for a few seconds, and then exhale. It was so incredibly hard because it hurt my stomach so badly. Anytime my mother got it out (I was supposed to do it about 10 times a day) I would begin crying and refuse to do it. But it was crucial. I had begun to build up fluid in my lungs and this was the way to get rid of it. My poor mother. I remember her crying, holding my face, telling me, "I'm not going to lose you to pneumonia when you're sitting here with cancer!" After seeing how much she was hurting over this, I sucked it up (literally) and did my breathing exercises (which continued all 14 days in the hospital and all throughout my weeks of recovery at home.)
This surgery was also the start of my ridiculous anxiety. It became really, really bad. I never wanted my mom to leave. She would sleep in the waiting room (because people were not allowed in our hospital rooms after visiting hours), or sometimes they were nice enough to let her sleep in my room, as long as my roommate didn't mind. My mom would go home to shower while someone else (family or friend) was sitting with me. She would leave and I'd get anxious. Then, it would be so bad and I'd call her, asking how long until she had returned. Usually, she hadn't even made it home at that point. My poor mother. I'm sure my anxiety and constant wanting her by my side only made things that much harder for her. She lived at the hospital with me for 14 days. Rarely went home. Rarely slept (because how can you in an uncomfortable chair?). When she slept in the waiting room, I'd call her multiple times a night, asking her to come to my room. But she never once complained. She was so incredibly strong for me.
Throughout my stay, I had many tests ran. I had ultrasounds done on my legs and groin area to make sure I didn't have any clots from not getting up and walking around. Although I had compression stockings on that tightened and loosened every few minutes (much like a blood pressure cuff) to help with circulation, blood clots from lack of movement were still a risk.
I had a few x-rays while there but those were always done in my bed. They'd come in around 2am, slip a board under my back, wheel a giant machine in, do the x-ray and leave.
I also had many, many vials of blood drawn and tested.
The worst of my tests was the barium swallow. They wheeled me down to a bottom floor of the hospital. I sat in the wheelchair for far too long, growing weak, nauseous, and anxious. They finally took me back into the examine room. There was a large table that they wanted me to crawl on. I explained to them that this was not going to be possible because I could not use my abdomen. Two techs stood there, contemplating different ways to get me on the table. When standing, it hit me around my hips. Finally, they got a step stool. At this point, I had grown far too weak. I really don't remember how, but somehow I got on the table. They put straps all over me so that I didn't need to use any energy to hold myself up. Then the table began moving into odd positions and I was asked to swallow this nasty, thick liquid. The barium swallow basically watched how my mouth, esophagus, and stomach all functioned. This was necessary before I could be discharged and allowed to eat on my own. It was a horrific procedure and by the end, I was in tears and so much pain. I had never been so happy to be back in a hospital bed as I was at the end of this.
After about 10 days in the hospital, Dr. Linehan came into my room after one of my PT sessions. I was sitting in the chair at the foot of my bed. He leaned against the end of the bed and it was difficult for him to make eye contact with us. He then informed us that they were wrong about me having GIST. He said my last c-kit stain came back negative, indicating I had Leiomyosarcoma. At the time, my mother and I knew nothing about it. We couldn't even pronounce it and asked him to write it down for us. He then explained that Washington University (where I was) didn't believe this diagnosis. So they tested it again. To get the same results. They still weren't certain to they sent it to Sloan-Kettering, another top hospital in the northeast. And they too, were highly shocked and confused, but also confirmed the Leiomyosarcoma diagnosis.
We didn't know what to think. But judging by Dr. Linehan's glassy eyes, his lack of eye contact, and his almost defeated demeanor, we knew it wasn't good. I knew enough about cancers to know that "sarcomas" are bad. They're some of the worst and rarest out there. Dr. Linehan informed us that it is a very, very rare cancer. That only four in one million people get it. That it's aggressive and severe (hence why it grew so quickly.) He said typically, removal is the only treatment. But that my tumor tested highest grade (meaning the cancer cells were dividing at the most rapid rate he had ever seen) and this gave them strong reason to believe the cancer cells had entered my bloodstream, and were now looking for a new place to attach to and grow. He promised me he would set me up with the best oncologists there were and he promised to get me the best care possible. He also said he was going to present my case to the oncology board of experts that he meets with every Monday of the month and they would devise the best radiation and chemotherapy treatment plan for me. Before he left, he advised us to stay away from the internet. "The things you read will only scare you. And your case isn't the typical case. Most Leiomyosarcoma patients are 50+ years old and it occurs in their extremities. You are 21 and it was in your stomach. You don't fit the standard so you can't compare yourself to what you read." And we took his advice. My mother and I stayed off the internet. (Too bad we couldn't convince my father of this. He immediately took to the internet and didn't heed the doctors warning. He read it all and thought it applied to me and became very scared and worried.)
Dr. Linehan told us to contact him anytime we needed him and told me to stay strong. When he left the room, I broke down. For the first time, I realized what this all meant. I had cancer. It hadn't truly sunk in though. But I kept repeating in my head "I don't want to die." Dr. Linehan's reaction had me so worried. He deals with this on a daily basis. Why was this so hard for him to tell us? ...."because it's so bad" is what I thought. But I didn't realize just how right I was.
A few days before leaving the hospital, I needed my drains to be taken out. One afternoon, one of Dr. Linehan's residents came in to take the tubes out. I asked if it would hurt and he said no. He took the bandages off the site where the tubes entered my stomach, cut the stitches holding them in, grabbed them in one hand, then said, "I'm going to count to three." But he lied. On two, he yanked them out and I screamed the loudest I've ever screamed in my life!!!! (And I have a very high pain tolerance, especially at this point). As they came flying out, they were making this nasty gushing noise. Blood and yellow liquid were all over his white coat, the side of the bed, etc. He apologized and explained that if he had said it would hurt, I would have tensed and made it more painful. (Which is true but still made me mad). He then explained the tubes actually get bigger as they go in, so that's why it was so painful. After he left, I told my mother, "This feeding tube is staying in the rest of my life. I am NOT going through that again."
I had amazing nurses while in the hospital and I had horrible nurses. Some truly cared, and others were just there for a paycheck. During surgery, I started my period. It's common for this to happen during a traumatic event to your body. However, very few nurses cared for this matter. They would seriously just leave me in a pad all day (No tampons allowed). My mother was the one who changed it and cleaned me. Ridiculous!!!
Cleanliness was also an issue. One evening, my mother mentioned to a nurse that I hadn't had a bath in days. This nurse was disgusted and told my mother that late that night, when things were calmer and patients were sleeping, she would be in to bathe me. This amazing nurse came in, helped move me to a chair and thoroughly cleaned my body. I cannot tell you how much better I felt.
On other days, a nurse would come in the room, set a bucket of lukewarm water down on a table, with soap and a rag and say "You can take a sponge bath" and closed the curtain. Did these people read my chart???? Did they not know I could barely get out of bed, let alone sponge bathe myself? One nurse, I even told I can't do this alone and she shrugged and walked out. I called my mother crying. She would immediately come in from wherever she was (home, the cafeteria, the waiting room doing work, etc) and bathe me. It's the poor excuse for nurses like them that made me want to go into nursing to make sure people had a nurse they could count on. One that truly cared.
I remember there were students working on our floors. One was assigned to a patient for a day. I had a student, maybe only 5 years older than me, that was so sweet. She was so thorough and so attentive. That afternoon she asked, "If you could have anything, what would it be." I said "my hair washed. It hasn't been washed since the night before my surgery." (Which was well over a week ago). She left the room and came back with a giant bucket of water, some shampoos, cups and sponges. She moved my bed out from the wall, helped me move my body towards the top of the bed, and hung my head off the bed. She covered the ground with towels and began pouring water all over my head, letting it fall into the bucket (and half of it on the floor) and she massaged my head with shampoo for a good 10 minutes. I cannot begin to tell you how much I appreciated this. It sounds silly but having my hair washed made me feel a million times better (especially because I had so many people coming in and visiting me). I wish I could remember her name to contact her and thank her. She and the one that bathed me are the exact type of nurse I want to be.
I remember each day I grew anxious and hopeful that I would be discharged. And each day I was told "one more day". I became so discouraged thinking I was going to stay in that hospital forever. After exactly 14 days in the hospital, and much begging on my part, I was discharged to go home. I know it was only 14 days, but it seriously felt like 3 months to me!
Dr. Linehan's care and concern throughout this all is what makes him one of the best doctors ever. I could see through his pain of giving us the bad news, that I wasn't just a patient to him. He truly cared about me. And he made good on his promise. Before I was discharged from the hospital, he had referred me to two of the best oncologists to set up appointments once he had met with the board of experts.
He informed us that he would most likely have to crack my chest and that he would be removing my entire stomach. He would then cut a piece of my small intestine or colon and create a stomach out of that. It was a rare surgery but he is one of the top in the nation and we trusted him. He briefly mentioned I'd be on bedrest for a while after surgery but never really mentioned just how painful recovery would be.
Late afternoon on February 13, 2006, my brother, sister, and I all piled in the car and headed to St. Louis. I remember my mother being so mad because we got on the road much later than we planned, and I needed to be home to drink my nasty drink to completely clear out my digestive system.
We arrived home around 8pm, I drank my drink, and honestly, didn't expel of much like I was told I would.
I went to sleep that night without a care in the world. I really wasn't concerned. I didn't think I needed to be. My tumor was benign and for some reason, I was under the impression this was going to be a simple surgery. Looking back, I'm not at all sure why I thought this. Had I not heard the doctor say they were going to crack my chest and remove my stomach? Honestly, I think I was just relieved to know my tumor was benign so nothing else seemed to matter to me. I was just ready to get it all over with. Little did I know that this was my last night of lying down without worrying. Little did I know from that night forward, I'd worry so much.
The next morning, we headed to the hospital. My surgery wasn't slated until about 2pm that afternoon. I was shocked when shortly after arriving at 8am, they called my name to go up to pre-op. I wasn't expecting it. My siblings, Ben and Leah, had stopped at another hospital to see my Grandma who had just had a total knee replacement. They weren't there to see me off.
My mother asked if they could go with me and the staff said no. (Looking back, I'm not sure why. I went to the exact same pre-op I have been going to for years now afterwards for my endoscopies and they ALWAYS let someone come with me.)
My mom and dad teared up, hugged me tight, told me they loved me, and that they'd see me soon. I remember feeling weird. Should I be crying? My parents are. They seem so worried. Should I be? Have I been in denial over what's really happening? Maybe I didn't prepare for this like I should have. As I was walking back to the elevator to be taken up to pre-op I became so scared and sick to my stomach. I suddenly realized this was a bigger deal than I thought. I wasn't going in for a simple surgery. My parents were crying for a reason. And I was now alone.
In pre-op, I was overwhelmed. I had never been in this situation. They asked me so many medical questions. I didn't have a medical history prior to this. And everything in the past few weeks was new and confusing. I didn't even know the answer to half of the questions. I wanted my parents with me so badly. I needed their help with these questions. I changed into a gown, and was hooked up to an IV. I had a ridiculous amount of doctors and nurses and PAs coming in. My surgeon came in, then his residents, then his nurse, then his physician's assistant. Then the anesthesiologist came in, then their nurse, then their residents. So many people. All asking the same questions. And everyone was just so interested in my rare story. After the fourth "You're too young to be going through all of this", I started to get anxious out of fear of what "this" was.
Thankfully, I began to calm down as I realized I was in very good hands. All the questions were answered, urine sample given (they refused to believe I was a virgin and demanded a pregnancy test. I guess it's hard to believe a 21 year old is still a virgin these days???) I was just chilling in the bed, wrapped in blankets, with saline running through my body.
Then the anesthesiologist came in. They asked if I wanted an epidural. 'Epidural?? I'm not having a baby' I thought. Until this point, all things health and medical were not interesting to me. Actually, all things medical related made me queasy. I had only ever heard of an epidural in relation to pregnancy. I had no idea that it blocked pain. (Looking back, I was stupid. I should have known that but it just goes to show so how far removed I was from this all.) When they asked, I looked at them, with a terrified face, and said "I don't know. Do I need one?" The anesthesiologist's face instantly changed demeanors, as if saying "this poor girl" and she grabbed my hand and said very slowly and softly, "Honey, you're getting a very major surgery. I'm sorry there's no one up here with you, but yes, I would highly, highly recommend an epidural." I began crying, agreed to the epidural, and signed a form after being read the risks involved. Then they came in, told me to sit up, swing my legs off the side of the bed. They brought over a table, placed a pillow on top, and told me to lean forward over the pillow. I saw the ginormous needle and began (internally) freaking out. It hurt so badly!!!!!!! I began crying and asked if there was any way my mom could come up. Unfortunately, we were close to surgery time so they said no. (I've never seen more people look so sorry for something than the staff did for me on that day.)
Shortly after, an anesthesiologist came in and said they were going to give me something to relax me and then I'd be taken back to the operating room. Whatever they gave me made me feel drunk. But definitely relaxed. Things became a blur. I remember being wheeled down the long hallway into the OR. At this point, I was out of it enough that I couldn't open my eyes or speak, but I could still hear things around me and was conscience of what was going on.
They peeled off my gown, exposing my entire front side down about 6 inches past my belly button. They began cleaning my entire body...my neck, my entire chest, my stomach, and down past my belly button. I remember being so incredibly cold (those ORs are FREEZING to begin with. Then add in the fact that you're now wet and fully exposed, it's horrible.) They then just stood around talking, leaving me exposed (they couldn't cover me up because they had just sterilized my entire body) for what felt like 10 minutes. I felt so awkward. Just lying there, face up, topless, freezing cold. Finally, I heard Dr. Linehan enter. They placed a mask on my face, the anesthesiologist then said they were going to give me the drug to knock me out and asked me to count backwards from 10. I made it to 8 and I was out.
The surgery took about 6 hours. Afterwards, Dr. Linehan came down to the waiting area and pulled my family into a consult room. (At that time, my mother, father, brother, sister, grandpa and a few aunts and uncles) were all there. He explained that the surgery went well and because the tumor was encapsulated, he was able to save two-thirds of my stomach and only removed the very top third, plus the very bottom of my esophagus. I was also fortunate that he was able to work around my ribs and they did not have to be cracked. Then came the bad news. He told my family that the pathologist would confirm it, but their original tests were wrong. My tumor was in fact malignant. They were also informed the tumor, in just three short weeks, had grown from the size of a golf ball, to the size of an orange. (I cannot imagine how large it would have been if we had not been offered this cancelation in his schedule and kept our original April date.)
I had been cut from just below my sternum, down to about an inch-and-a-half above my belly button. I had a feeding tube on my right side that went directly into my small intestine. I had a drain on my right side (I'm not sure where it went into. I'm pretty sure it was my stomach.) Thankfully, Dr. Linehan had an AMAZING resident working with him, Dr. Doyle. She asked Dr. Linehan if she could stitch me up herself, explaining that I was far too young, with far too nice of stomach to have a big ugly scar. She took her time and spent more than double the time that most people would take to stitch someone up.
I was in recovery in the ICU. I will say that I do not remember much of my first 9 days (of 14) that I was in the hospital. I have very few, very blurry memories. My first memory, I was lying in the bed, not too long after surgery, and I could sense an elephant in the room. Even though I was told before my surgery that my tumor was benign, I could sense that had changed. I asked my brother, "Do I have cancer?" To which my mother responded "Yes." And then I freaked out. Sobbing. My machines all started going crazy and the nurses had to come in and calm me. I cannot imagine being my family, having to find this out, then tell me, and watch my reaction, while already watching me in so much pain.
During these first three days, my pain was not manageable. When the doctors would ask on a pain scale from 1 to 10, with 10 being hit by a semi-truck, how did I feel, I would always say a 10. I was always crying. Always in so much pain. I was on the highest dose of pain medication. They could not give me anymore without me becoming toxic. My original surgery was on Tuesday and just a few days later on Friday, Dr. Linehan decided to take me back in for surgery. He said there was no reason I should still be in that amount of pain and I could possibly have an infection or something such as a sponge may have been left in me.
Thankfully, after reopening me, they saw nothing. Dr. Linehan flushed me out, added another drain to my side, and I was closed back up. Again, Dr. Doyle took her time stitching me up. I cannot thank her enough. I've seen too many scars in my days (many of them other places on my body now) and they look large, rough, puffy in places. The scar on my stomach looks absolutely amazing. Honestly, I don't know that for as large a cut as was made, that it could look any better. I truly appreciate her genuine character for wanting to do this for me. I am very insecure about my scars, especially that one, but I cannot imagine how much worse it would be had any other doctor stitched me up.
Anyway, this second surgery seemed to do the trick because my pain had receded so much compared to the previous few days.
Dr. Linehan told us they thought my tumor was a GIST (gastro-intestinal stomal tumor). This was actually good news. With the cancers it could be, this was the best one. It was simply treated with a Gleevac pill, with none of the typical side effects of cancer (nausea, hair loss, fatigue, etc). And these cancers very rarely come back. We were very relieved to hear this and just needed to wait for the final pathology report to confirm it, before beginning treatment.
As I said, I do not remember much of my first 9 days in the hospital. I was not allowed to eat or drink ANYTHING. I wasn't even getting anything put into my feeding tube. I was simply living off whatever was going into my IVs. My mouth was so dry. My family members were allowed to wet a sponge and move it around my mouth to moisten it. I would cheat and squeeze it with my tongue and cheek to drink the water. But the moment it went down, the drains sucked it right out. It was frustrating because I just wanted to drink.
We also realized, while in ICU, that I am allergic to morphine. It causes itching and hallucinations. So much so that I was injuring myself. I would think I was a rollercoaster and it was headed for a wall, so I would jump out. But in reality, I was sitting up (using my abdomen which wasn't allowed) and trying to jump out of bed. My hallucinations kept causing me to move around which then caused a large deal of pain for me, and also caused me risk of injuring my surgery site. I was quickly taken off that.
Another side effects of the pain medicine was that it made me see things. They weren't hallucinations, more so just effects of the medicine. And they didn't cause me any physical pain. For instance, I would tell my brother that there were dinosaurs in my room. In reality, they were just flowers in vases. One time, I began swatting at the air asking my best friend, Jessie, "Do you see that?!" I thought I saw something falling all around me, and was swatting at it all. Another time, I yelled at my mother that someone was trying to come in the door behind me, when in fact, there was no door behind me, only a wall. Another time while Jessie was there, I was yelling at our cat, Mike Jones, to leave me alone. Jessie kept telling me he wasn't there but I saw him and he was bothering me. Thankfully, my family and friends saw humor in all of this.
In the hospital, I was not allowed to use my abdomen. At all. I just laid there in bed. After I was out of ICU, I began physical and occupational therapy. Physical therapy first started with learning to sit up. I had to grip the side rail of the bed with my arm, pull myself on my side, then push myself up with my arms, then lift my legs off the side of the bed. It might sound easy but it was so incredibly hard. You never truly realize how much you rely on your abdomen until you're not allowed to use it. Then I would learn to stand. Then to walk.
Occupational therapy worked with me to learn to put my socks on (another very difficult task since I was not allowed to bend over). They taught me how to use the restroom and how to do my breathing exercises.
Oh those breathing exercises. I hated them. I refused to do them. Essentially, I had this apparatus.
+(HD).jpeg) |
| via |
This surgery was also the start of my ridiculous anxiety. It became really, really bad. I never wanted my mom to leave. She would sleep in the waiting room (because people were not allowed in our hospital rooms after visiting hours), or sometimes they were nice enough to let her sleep in my room, as long as my roommate didn't mind. My mom would go home to shower while someone else (family or friend) was sitting with me. She would leave and I'd get anxious. Then, it would be so bad and I'd call her, asking how long until she had returned. Usually, she hadn't even made it home at that point. My poor mother. I'm sure my anxiety and constant wanting her by my side only made things that much harder for her. She lived at the hospital with me for 14 days. Rarely went home. Rarely slept (because how can you in an uncomfortable chair?). When she slept in the waiting room, I'd call her multiple times a night, asking her to come to my room. But she never once complained. She was so incredibly strong for me.
Throughout my stay, I had many tests ran. I had ultrasounds done on my legs and groin area to make sure I didn't have any clots from not getting up and walking around. Although I had compression stockings on that tightened and loosened every few minutes (much like a blood pressure cuff) to help with circulation, blood clots from lack of movement were still a risk.
I had a few x-rays while there but those were always done in my bed. They'd come in around 2am, slip a board under my back, wheel a giant machine in, do the x-ray and leave.
I also had many, many vials of blood drawn and tested.
The worst of my tests was the barium swallow. They wheeled me down to a bottom floor of the hospital. I sat in the wheelchair for far too long, growing weak, nauseous, and anxious. They finally took me back into the examine room. There was a large table that they wanted me to crawl on. I explained to them that this was not going to be possible because I could not use my abdomen. Two techs stood there, contemplating different ways to get me on the table. When standing, it hit me around my hips. Finally, they got a step stool. At this point, I had grown far too weak. I really don't remember how, but somehow I got on the table. They put straps all over me so that I didn't need to use any energy to hold myself up. Then the table began moving into odd positions and I was asked to swallow this nasty, thick liquid. The barium swallow basically watched how my mouth, esophagus, and stomach all functioned. This was necessary before I could be discharged and allowed to eat on my own. It was a horrific procedure and by the end, I was in tears and so much pain. I had never been so happy to be back in a hospital bed as I was at the end of this.
After about 10 days in the hospital, Dr. Linehan came into my room after one of my PT sessions. I was sitting in the chair at the foot of my bed. He leaned against the end of the bed and it was difficult for him to make eye contact with us. He then informed us that they were wrong about me having GIST. He said my last c-kit stain came back negative, indicating I had Leiomyosarcoma. At the time, my mother and I knew nothing about it. We couldn't even pronounce it and asked him to write it down for us. He then explained that Washington University (where I was) didn't believe this diagnosis. So they tested it again. To get the same results. They still weren't certain to they sent it to Sloan-Kettering, another top hospital in the northeast. And they too, were highly shocked and confused, but also confirmed the Leiomyosarcoma diagnosis.
We didn't know what to think. But judging by Dr. Linehan's glassy eyes, his lack of eye contact, and his almost defeated demeanor, we knew it wasn't good. I knew enough about cancers to know that "sarcomas" are bad. They're some of the worst and rarest out there. Dr. Linehan informed us that it is a very, very rare cancer. That only four in one million people get it. That it's aggressive and severe (hence why it grew so quickly.) He said typically, removal is the only treatment. But that my tumor tested highest grade (meaning the cancer cells were dividing at the most rapid rate he had ever seen) and this gave them strong reason to believe the cancer cells had entered my bloodstream, and were now looking for a new place to attach to and grow. He promised me he would set me up with the best oncologists there were and he promised to get me the best care possible. He also said he was going to present my case to the oncology board of experts that he meets with every Monday of the month and they would devise the best radiation and chemotherapy treatment plan for me. Before he left, he advised us to stay away from the internet. "The things you read will only scare you. And your case isn't the typical case. Most Leiomyosarcoma patients are 50+ years old and it occurs in their extremities. You are 21 and it was in your stomach. You don't fit the standard so you can't compare yourself to what you read." And we took his advice. My mother and I stayed off the internet. (Too bad we couldn't convince my father of this. He immediately took to the internet and didn't heed the doctors warning. He read it all and thought it applied to me and became very scared and worried.)
Dr. Linehan told us to contact him anytime we needed him and told me to stay strong. When he left the room, I broke down. For the first time, I realized what this all meant. I had cancer. It hadn't truly sunk in though. But I kept repeating in my head "I don't want to die." Dr. Linehan's reaction had me so worried. He deals with this on a daily basis. Why was this so hard for him to tell us? ...."because it's so bad" is what I thought. But I didn't realize just how right I was.
A few days before leaving the hospital, I needed my drains to be taken out. One afternoon, one of Dr. Linehan's residents came in to take the tubes out. I asked if it would hurt and he said no. He took the bandages off the site where the tubes entered my stomach, cut the stitches holding them in, grabbed them in one hand, then said, "I'm going to count to three." But he lied. On two, he yanked them out and I screamed the loudest I've ever screamed in my life!!!! (And I have a very high pain tolerance, especially at this point). As they came flying out, they were making this nasty gushing noise. Blood and yellow liquid were all over his white coat, the side of the bed, etc. He apologized and explained that if he had said it would hurt, I would have tensed and made it more painful. (Which is true but still made me mad). He then explained the tubes actually get bigger as they go in, so that's why it was so painful. After he left, I told my mother, "This feeding tube is staying in the rest of my life. I am NOT going through that again."
I had amazing nurses while in the hospital and I had horrible nurses. Some truly cared, and others were just there for a paycheck. During surgery, I started my period. It's common for this to happen during a traumatic event to your body. However, very few nurses cared for this matter. They would seriously just leave me in a pad all day (No tampons allowed). My mother was the one who changed it and cleaned me. Ridiculous!!!
Cleanliness was also an issue. One evening, my mother mentioned to a nurse that I hadn't had a bath in days. This nurse was disgusted and told my mother that late that night, when things were calmer and patients were sleeping, she would be in to bathe me. This amazing nurse came in, helped move me to a chair and thoroughly cleaned my body. I cannot tell you how much better I felt.
On other days, a nurse would come in the room, set a bucket of lukewarm water down on a table, with soap and a rag and say "You can take a sponge bath" and closed the curtain. Did these people read my chart???? Did they not know I could barely get out of bed, let alone sponge bathe myself? One nurse, I even told I can't do this alone and she shrugged and walked out. I called my mother crying. She would immediately come in from wherever she was (home, the cafeteria, the waiting room doing work, etc) and bathe me. It's the poor excuse for nurses like them that made me want to go into nursing to make sure people had a nurse they could count on. One that truly cared.
I remember there were students working on our floors. One was assigned to a patient for a day. I had a student, maybe only 5 years older than me, that was so sweet. She was so thorough and so attentive. That afternoon she asked, "If you could have anything, what would it be." I said "my hair washed. It hasn't been washed since the night before my surgery." (Which was well over a week ago). She left the room and came back with a giant bucket of water, some shampoos, cups and sponges. She moved my bed out from the wall, helped me move my body towards the top of the bed, and hung my head off the bed. She covered the ground with towels and began pouring water all over my head, letting it fall into the bucket (and half of it on the floor) and she massaged my head with shampoo for a good 10 minutes. I cannot begin to tell you how much I appreciated this. It sounds silly but having my hair washed made me feel a million times better (especially because I had so many people coming in and visiting me). I wish I could remember her name to contact her and thank her. She and the one that bathed me are the exact type of nurse I want to be.
I remember each day I grew anxious and hopeful that I would be discharged. And each day I was told "one more day". I became so discouraged thinking I was going to stay in that hospital forever. After exactly 14 days in the hospital, and much begging on my part, I was discharged to go home. I know it was only 14 days, but it seriously felt like 3 months to me!
Dr. Linehan's care and concern throughout this all is what makes him one of the best doctors ever. I could see through his pain of giving us the bad news, that I wasn't just a patient to him. He truly cared about me. And he made good on his promise. Before I was discharged from the hospital, he had referred me to two of the best oncologists to set up appointments once he had met with the board of experts.
Friday, March 1, 2013
Recovery
For days, I begged my doctor, Dr. Linehan, to let me go home. After 14 days in the hospital, I was finally being discharged.
My mother and father loaded my Dad's car up with all the balloons, flowers, cards, and gifts. Then my mom pulled her car up to the front of the hospital, they wheeled me out in a wheelchair and I climbed inside. Mom tried to drive so carefully, but the 40 minute car ride home was horrendous. Every tiny bump hurt my abdomen so badly, causing me to cry.
Once home, I started to freak out (on the inside as to not upset my mother, but I'm sure she was having these same thoughts.) I realized that I no longer had professional care. When my pain became too bad, when I was nauseous, when I had questions, etc. I could no longer press a call button and have someone at my bedside in a matter of minutes to take care of the problem. Yes, my mom was at my side within seconds of needing her, but we were confused. Medical issues were far from our area of expertise. Will we know what to do?? What if something goes wrong?? Hospitals makes things so much easier by administering medications directly to you at your bedside.
Thankfully, things went as well as they could without professional help there 24/7.
After two weeks of no abdomen use in the hospital, that same course of recovery continued at home. I was not allowed to use my abdomen for the next 10 weeks.
I was also not allowed to lift anything over 5 pounds. This was annoying for me because anytime I needed anything, even my laptop (they weren't made super thin back then), I would need to call for assistance. A few times, my stubbornness took over and I refused to ask for help. This resulted in a dropped laptop (and dented laptop) and excruciating pain.
Once home, I was finally allowed to eat normal table food. However, my body couldn't consume a lot in one sitting since my stomach was now so small from the surgery that removed one-third of it and also from not eating for 2 weeks in the hospital. For breakfast, Mom would make me a pancake, about the size of a half dollar. Even that was too much. It filled me too quickly. Trying to eat and stretch my stomach out was painful and left me in tears everyday. My mother would get frustrated (yet hide it well) because she knew it was important for me to eat and maintain my weight, but she also felt bad forcing me to do something that hurt me so badly.
Because I was still not eating much, we continued to use my feeding tube throughout the night. Around 10pm, we'd clean it out, extract all the air from the tubing, and hook it up to my feeding tube. We'd then pour two full cans of Boost or Ensure into the bag hung on my IV pole. Over the course of the next 10-12 hours, the supplement would slowly enter my small intestine, providing me with nutrients needed to keep me alive, strong, and maintain my weight. (Huge thanks to the American Cancer Society that provided one free case a month to cancer patients via the Hope Lodge! It truly helped out budget!)
A side effect of the surgery was intense right shoulder pain. At times, this pain was much more excruciating than my stomach pains. We called the doctor numerous times over it and they proscribed more pain meds, but honestly, they didn't seem to help. I was constantly screaming and crying out in pain. There is a nerve that runs from your diaphragm to your shoulder, and it was a "related" pain I was experiencing During surgery, things in my abdomen were shifted a little bit to perform the extraction of my tumor, part of my stomach, and part of my esophagus. This was the cause of my shoulder pain. By the end of the 10 weeks of recovery at home, it had gotten much better, but it didn't completely disappear until about 6 months out from surgery. Even years later, I will still experience this pain every few months when I'm using my abdomen or have used it a lot that day.
Showering was a difficult task. Because I could not bend over, I was not able to properly clean myself. All modesty went out the window at this point. I would get in the shower and wash my hair and upper body. But when it came time to anything below my waist, I would need assistance. I'd yell for my mom, turn the shower head away from the end of the shower, and she'd open the shower curtain and wash the rest of my body and shave my legs for me. Mom of a Lifetime Award right there!!! Thankfully, she was completely used to caring for me in this way because of the nurses lack of care in the hospital during recovery.
During my recovery, my anxiety became far worse than it was in the hospital. At the hospital, I just wanted my mother around 24/7. Thankfully, for her sake, that subsided. But it was replaced by a tense, shaky body. Part of it was due to withdrawal symptoms as I weaned myself off the pain medication, but the majority of it was anxiety. I would lay in bed and watch the hours pass...midnight, 1am, 2am, 3am, and so on. Many, many days my mother would sit up with me and I wouldn't fall asleep until about 6am. I just sat there, shaking, nervous, and incredibly anxious. Honestly, anxiety is hard to describe. Because a lot of the time, it's not a physical thing. It's a mental thing. I just sat there freaking out. My main physical symptom, weird as it was, was my hands. I could NOT close them. They were open, fingers as straight, tense, and locked as they could be. I couldn't close them because if I did, I would FREAK OUT and start going crazy.
Many nights, around 4:30am, my mom would get out of bed, bundle me up (because it was about 20 degrees outside) and make me take a walk throughout the neighborhood. She thought fresh air and getting out of my confined house would help. Most of the time it did. I would come back calmer and able to sleep.
I cannot thank my mother enough for those countless weeks where she sat up with me throughout the night. Especially because she would have to work the next day (thank goodness she had a job that she worked from home!). Looking back, I don't know how my mother didn't fall apart having to deal with me and function on so little sleep. Sure, I functioned on little sleep, but all I did all day was lay around. She had to work, make meals, clean, take care of me, etc. She is a superhero for sure!
There is really no way to convey how difficult this time was for me. I was in the worst pain of my life. My doctor had warned me that this type of surgery is one of the most painful to recover from. And that mine would be even more painful, and longer than average, because of the amount of muscle I had. He informed me that muscle is not only more painful to repair, but it takes longer. He then gave me (what I can now see as a compliment but didn't then) some bad news. He had never seen anyone with the amount of abdominal muscles as I had. He was shocked that there was no fat, but just lots and lots muscle. While this sounds great on the surface, it meant that my recovery would be incredibly painful and take even longer. Lucky me =/
And he was right. Recovery was horrendous. The pain from my stomach is unfathomable. The pain from my shoulder was unmangeable. I couldn't eat much and it hurt to do so. I was anxious. I was emotionally beaten. I was so scared for my future...or wondering if I'd even have a future.
Everyone thinks I am so strong. The truth is, I didn't possess this strength in the first 8 weeks at home. I was far beyond weak. As I said, I cannot begin to express the pain I was in. It was so bad that I wanted to give up. I wanted to die. I told my mother that I couldn't take it anymore. To just let me be. To let me go. That death would be far better than the pain I was experiencing. Looking back, I cannot imagine how hard this was for her to hear. She grabbed my face in her hands and through tears said she would not allow for that to happen. And she didn't. She remained so incredibly strong for me when I was so incredibly weak. SHE is the reason I am here today. She wouldn't let me give up even when I wanted to leave this earth.
Around my 8th week at home, I went back to Dr. Linehan to get my feeding tube sewn back in (your body rejects foreign objects, so over the course of time, my body pushed the stitches out, until they ripped through the top layer of skin, leaving nothing holding my feeding tube in.) While at my appointment, I mentioned how down and beaten I felt; the pain I was in.
He said something that completely changed my outlook on this all.
"You can't let it consume you. The ones who don't make it are the ones who let it consume them and ruin their life." It scared me. But that's what I needed. I decided right then and there to be strong. I had to be. I would not let cancer consume my thoughts and my life. I refused to lose this battle. I'd always heard "Attitude is half the battle" but I didn't TRULY understand it until now. Looking back, he was exactly right. My attitude, outlook, strength, and drive are definitely reasons why I am here today.
My mother and father loaded my Dad's car up with all the balloons, flowers, cards, and gifts. Then my mom pulled her car up to the front of the hospital, they wheeled me out in a wheelchair and I climbed inside. Mom tried to drive so carefully, but the 40 minute car ride home was horrendous. Every tiny bump hurt my abdomen so badly, causing me to cry.
Once home, I started to freak out (on the inside as to not upset my mother, but I'm sure she was having these same thoughts.) I realized that I no longer had professional care. When my pain became too bad, when I was nauseous, when I had questions, etc. I could no longer press a call button and have someone at my bedside in a matter of minutes to take care of the problem. Yes, my mom was at my side within seconds of needing her, but we were confused. Medical issues were far from our area of expertise. Will we know what to do?? What if something goes wrong?? Hospitals makes things so much easier by administering medications directly to you at your bedside.
Thankfully, things went as well as they could without professional help there 24/7.
After two weeks of no abdomen use in the hospital, that same course of recovery continued at home. I was not allowed to use my abdomen for the next 10 weeks.
I was also not allowed to lift anything over 5 pounds. This was annoying for me because anytime I needed anything, even my laptop (they weren't made super thin back then), I would need to call for assistance. A few times, my stubbornness took over and I refused to ask for help. This resulted in a dropped laptop (and dented laptop) and excruciating pain.
Once home, I was finally allowed to eat normal table food. However, my body couldn't consume a lot in one sitting since my stomach was now so small from the surgery that removed one-third of it and also from not eating for 2 weeks in the hospital. For breakfast, Mom would make me a pancake, about the size of a half dollar. Even that was too much. It filled me too quickly. Trying to eat and stretch my stomach out was painful and left me in tears everyday. My mother would get frustrated (yet hide it well) because she knew it was important for me to eat and maintain my weight, but she also felt bad forcing me to do something that hurt me so badly.
Because I was still not eating much, we continued to use my feeding tube throughout the night. Around 10pm, we'd clean it out, extract all the air from the tubing, and hook it up to my feeding tube. We'd then pour two full cans of Boost or Ensure into the bag hung on my IV pole. Over the course of the next 10-12 hours, the supplement would slowly enter my small intestine, providing me with nutrients needed to keep me alive, strong, and maintain my weight. (Huge thanks to the American Cancer Society that provided one free case a month to cancer patients via the Hope Lodge! It truly helped out budget!)
A side effect of the surgery was intense right shoulder pain. At times, this pain was much more excruciating than my stomach pains. We called the doctor numerous times over it and they proscribed more pain meds, but honestly, they didn't seem to help. I was constantly screaming and crying out in pain. There is a nerve that runs from your diaphragm to your shoulder, and it was a "related" pain I was experiencing During surgery, things in my abdomen were shifted a little bit to perform the extraction of my tumor, part of my stomach, and part of my esophagus. This was the cause of my shoulder pain. By the end of the 10 weeks of recovery at home, it had gotten much better, but it didn't completely disappear until about 6 months out from surgery. Even years later, I will still experience this pain every few months when I'm using my abdomen or have used it a lot that day.
Showering was a difficult task. Because I could not bend over, I was not able to properly clean myself. All modesty went out the window at this point. I would get in the shower and wash my hair and upper body. But when it came time to anything below my waist, I would need assistance. I'd yell for my mom, turn the shower head away from the end of the shower, and she'd open the shower curtain and wash the rest of my body and shave my legs for me. Mom of a Lifetime Award right there!!! Thankfully, she was completely used to caring for me in this way because of the nurses lack of care in the hospital during recovery.
During my recovery, my anxiety became far worse than it was in the hospital. At the hospital, I just wanted my mother around 24/7. Thankfully, for her sake, that subsided. But it was replaced by a tense, shaky body. Part of it was due to withdrawal symptoms as I weaned myself off the pain medication, but the majority of it was anxiety. I would lay in bed and watch the hours pass...midnight, 1am, 2am, 3am, and so on. Many, many days my mother would sit up with me and I wouldn't fall asleep until about 6am. I just sat there, shaking, nervous, and incredibly anxious. Honestly, anxiety is hard to describe. Because a lot of the time, it's not a physical thing. It's a mental thing. I just sat there freaking out. My main physical symptom, weird as it was, was my hands. I could NOT close them. They were open, fingers as straight, tense, and locked as they could be. I couldn't close them because if I did, I would FREAK OUT and start going crazy.
Many nights, around 4:30am, my mom would get out of bed, bundle me up (because it was about 20 degrees outside) and make me take a walk throughout the neighborhood. She thought fresh air and getting out of my confined house would help. Most of the time it did. I would come back calmer and able to sleep.
I cannot thank my mother enough for those countless weeks where she sat up with me throughout the night. Especially because she would have to work the next day (thank goodness she had a job that she worked from home!). Looking back, I don't know how my mother didn't fall apart having to deal with me and function on so little sleep. Sure, I functioned on little sleep, but all I did all day was lay around. She had to work, make meals, clean, take care of me, etc. She is a superhero for sure!
There is really no way to convey how difficult this time was for me. I was in the worst pain of my life. My doctor had warned me that this type of surgery is one of the most painful to recover from. And that mine would be even more painful, and longer than average, because of the amount of muscle I had. He informed me that muscle is not only more painful to repair, but it takes longer. He then gave me (what I can now see as a compliment but didn't then) some bad news. He had never seen anyone with the amount of abdominal muscles as I had. He was shocked that there was no fat, but just lots and lots muscle. While this sounds great on the surface, it meant that my recovery would be incredibly painful and take even longer. Lucky me =/
And he was right. Recovery was horrendous. The pain from my stomach is unfathomable. The pain from my shoulder was unmangeable. I couldn't eat much and it hurt to do so. I was anxious. I was emotionally beaten. I was so scared for my future...or wondering if I'd even have a future.
Everyone thinks I am so strong. The truth is, I didn't possess this strength in the first 8 weeks at home. I was far beyond weak. As I said, I cannot begin to express the pain I was in. It was so bad that I wanted to give up. I wanted to die. I told my mother that I couldn't take it anymore. To just let me be. To let me go. That death would be far better than the pain I was experiencing. Looking back, I cannot imagine how hard this was for her to hear. She grabbed my face in her hands and through tears said she would not allow for that to happen. And she didn't. She remained so incredibly strong for me when I was so incredibly weak. SHE is the reason I am here today. She wouldn't let me give up even when I wanted to leave this earth.
Around my 8th week at home, I went back to Dr. Linehan to get my feeding tube sewn back in (your body rejects foreign objects, so over the course of time, my body pushed the stitches out, until they ripped through the top layer of skin, leaving nothing holding my feeding tube in.) While at my appointment, I mentioned how down and beaten I felt; the pain I was in.
He said something that completely changed my outlook on this all.
"You can't let it consume you. The ones who don't make it are the ones who let it consume them and ruin their life." It scared me. But that's what I needed. I decided right then and there to be strong. I had to be. I would not let cancer consume my thoughts and my life. I refused to lose this battle. I'd always heard "Attitude is half the battle" but I didn't TRULY understand it until now. Looking back, he was exactly right. My attitude, outlook, strength, and drive are definitely reasons why I am here today.
Subscribe to:
Posts (Atom)